Abstract
INTRODUCTION Although pregnant people with sickle cell disease (SCD) are at increased risk of hypertensive disorders of pregnancy (HDP), no evidence informs what blood pressure thresholds to apply to diagnose HDP in people with SCD. HDP are typically defined by blood pressure 140/90 mmHg and laboratory abnormalities indicative of end-organ damage. However, people with SCD have lower baseline blood pressure compared to the general population. Thus, the existing HDP definitions potentially under-diagnose HDP in pregnant people with SCD, increasing the risk of significant HDP-related morbidity.
Early-onset preeclampsia develops prior to 34 weeks' gestation versus late-onset between 34 weeks and delivery. Early- and late-onset preeclampsia are believed to have distinct etiologic and prognostic significance and may be differently associated with blood pressure.
The objectives of our study were (1) to evaluate the sensitivity of various blood pressure thresholds in classifying preeclampsia in pregnant people with SCD, and (2) to determine whether the accuracy with which blood pressure thresholds classify pregnant people with preeclampsia differs between those with early- versus late-onset preeclampsia.
METHODS We reviewed all SCD pregnancies of at least 20 weeks' gestation that delivered at Mount Sinai Hospital, Toronto (1990-2017) or Johns Hopkins Hospital (2000-2021). We collected data on laboratory values, SCD complications, medication exposures, transfusion, delivery information, and fetal outcomes. We collected the highest systolic and diastolic blood pressure (SBP and DBP) in seven time periods: before pregnancy, at intake visit, 20-28 weeks' gestation, 28-34 weeks' gestation, last outpatient visit, at admission for birth, and six weeks postpartum.
New or worsening proteinuria (NWP) was defined as 0.3g/g on urine protein:creatinine ratio or 300mg on 24-hour collection; or, if a patient had baseline proteinuria, as doubling from baseline.
We compared the characteristics of pregnant people with NWP to those without. We then constructed receiver operating characteristic (ROC) curves to determine what SBPs and DBPs at the last outpatient visit most accurately classifies those with new or worsening proteinuria in SCD pregnancy. Finally, we divided patients with NWP into early- and late-onset and generated ROC curves for each group.
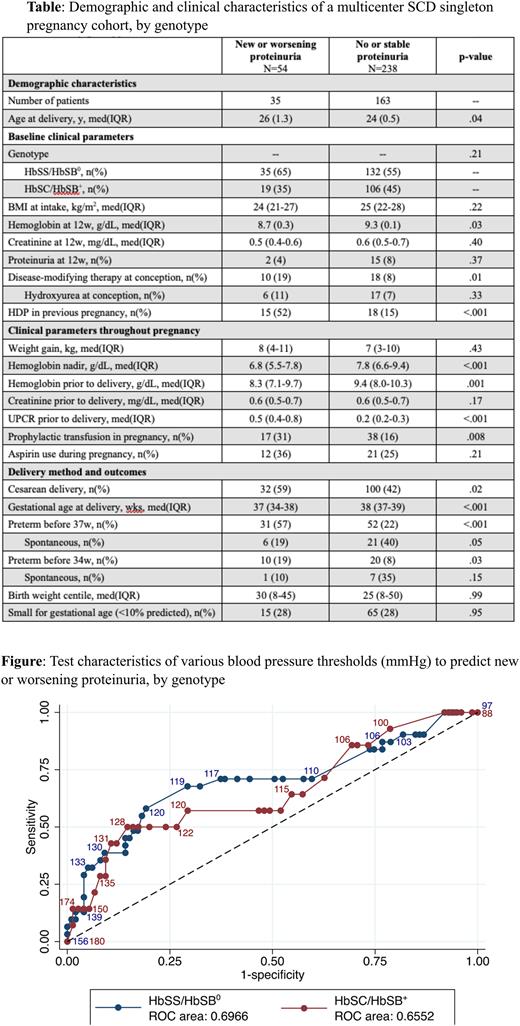
RESULTS We included 198 patients with 292 singleton pregnancies (Table). Fifty-four pregnancies had NWP. Of these, 24 (44%) were diagnosed with an HDP. NWP was associated with older age at delivery, higher rates of disease-modifying therapy at conception, higher rates of HDP in a previous pregnancy, and higher rates of preterm deliveries that were mostly attributable to induction of delivery. There was no difference in birth weight centile between the groups.
ROC curves indicate that blood pressure was modestly accurate at classifying those who developed NWP at any time after 20 weeks' gestation (Figure). For the cohort, the area under the curve (AUC) for SBP was 0.68 and for DBP was 0.63. Among those with HbSS/HbSβ0 the AUC for SBP was 0.70 and for DBP was 0.70. Among those with HbSC/HbSβ+ the AUC for SBP was 0.66 and for DBP was 0.53. Change in blood pressure from baseline was a poor predictor of NWP in both genotypes, with AUC<0.60 for SBP and DBP.
Using NWP as a traditionally-accepted standard for diagnosis of preeclampsia, the established threshold for HDP of 140/90 was 18% sensitive and 94% specific with a positive predictive value (PPV) of 44% and a negative predictive value (NPV) of 82%. In our sample, the optimal blood pressure cut-off was 120/70, which was 64% sensitive and 63% specific with a PPV of 31% and an NPV of 87%.
By timing of NWP onset, most (61%, n=33) had late-onset NWP. Blood pressure between 28 and 34 weeks' gestation did a poor job of classifying those who had early-onset NWP (AUC 0.44), while blood pressure between 34 weeks and delivery very accurately classified those who had late-onset NWP (AUC 0.82).
CONCLUSIONS Existing blood pressure thresholds used to diagnose HDPs are not sensitive in the SCD population. There is a need to consider lowering the BP threshold for HDP diagnosis among pregnant people with SCD. We propose a new threshold of 120/70, the adoption of which would improve identification of patients with SCD who need increased observation, consideration of early delivery, eclampsia prophylaxis, or possibly chronic transfusion therapy.
Disclosures
Malinowski:Alexion: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Pfizer: Consultancy. Kuo:bluebird bio: Consultancy; Apellis: Consultancy; Alexion: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; Pfizer: Consultancy, Research Funding; Celgene/BMS: Consultancy; Bioverativ/Sanofi/Sangamo: Membership on an entity's Board of Directors or advisory committees; Agios: Consultancy, Membership on an entity's Board of Directors or advisory committees. Pecker:Novo Nordisk: Consultancy; GBT: Research Funding; Global Blood Therapeutics: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal